Big news: Discharge is happening! I know the road is still going to be winding, but I am so happy that I’ll be able to sleep in a real bed. I haven’t been to the outside in 5 weeks!!!
Saturday, June 15, 2024 to Sunday, June 16, 2024 – Day 17 & 18
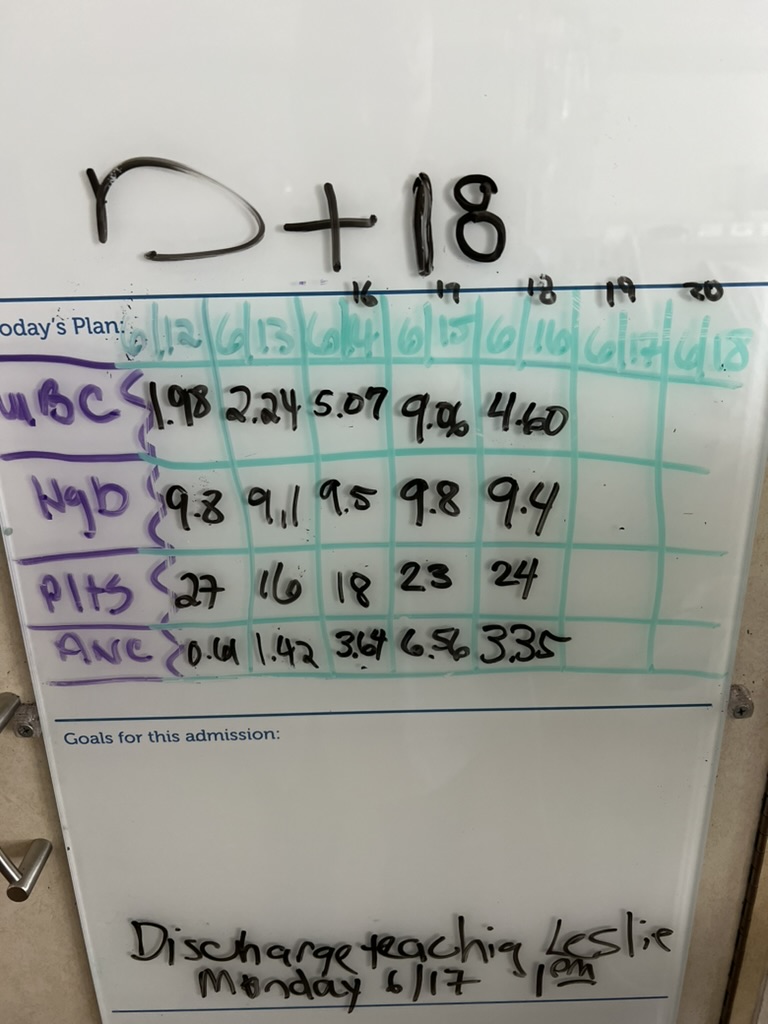
The weekend was an up and down. Saturday I felt pretty good and was able to eat 75% of my calories from real food (with the other 25% from my tube feed). I had spaghetti with meat sauce, rice and beans. I even went on two 15 minute walks around the floor which was the most I had done since I’ve been admitted to the hospital. However, I slept really poorly on Saturday night, probably because I discontinued one of my medications (olanzapine) so I was very groggy on Sunday and had to take two naps.
Despite feeling crummy on Sunday, I did finally transition all of my medications to oral, and I was able to eat 50% of my calories from real food and the other 50% from the tube feed. My IV pole looks a little empty these days, but I’m totally okay with that. It’s nice not having to go to the bathroom connected to this whole contraption.
Overall, the healing has not been linear. I thought that after counts came in, it’d just get better and better every day, but it’s been quite the opposite. Some days I feel like I can be a “normal” human; other days I still feel exhausted, nauseous, can’t walk more than 10 minutes.
Monday, June 17, 2024 – Day 19
I had my first solid stool today (yay), only to be followed by a “I need an emesis bag!!!” while still in the bathroom washing my hands. I had done a tube feed in the morning, so we decided that we’d stop them since I had been able to eat half of my calories off real food. Honestly, there’s no shame anymore being in the hospital – all bodily fluids, all ridiculous situations, are all fair game. The best thing to do is just laugh at it all after.
We had a two hour discharge teaching today with the nurse telling my family and me all about precautions for life outside of transplant. I can’t be in the sun. I can’t eat anything raw (no salads, no berries, etc.). I need to get up and walk around everyday even if I’m so exhausted. I’ll be at an apartment nearby the Bethesda area until day 100 because I still need to follow up in clinic 2 times a week. During the next 2.5 months, the team will continue to monitor my blood counts and ensure they’re trending in the right direction.
Tuesday, June 18, 2024 – Day 20
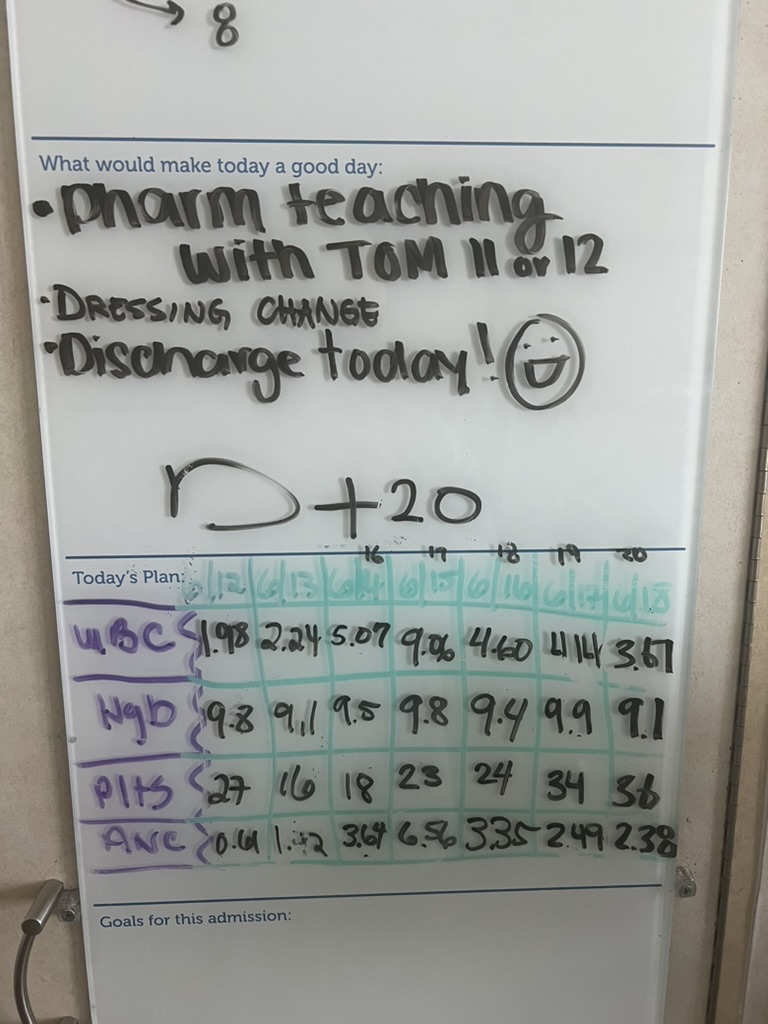
I’m getting discharged today! We were planning to discharge tomorrow, but given that it’s as holiday (Juneteenth) on Wednesday, we decided that Tuesday would be fine too and then I could come into clinic on Thursday. I’ve been joking that I’ve been in jail this whole time. It’s crazy to think that I haven’t been able to leave and see the outside since May 14th. It seems like it went by so quickly but at the same time, there were days that were so painful that I don’t even remember them (good thing for sedation).
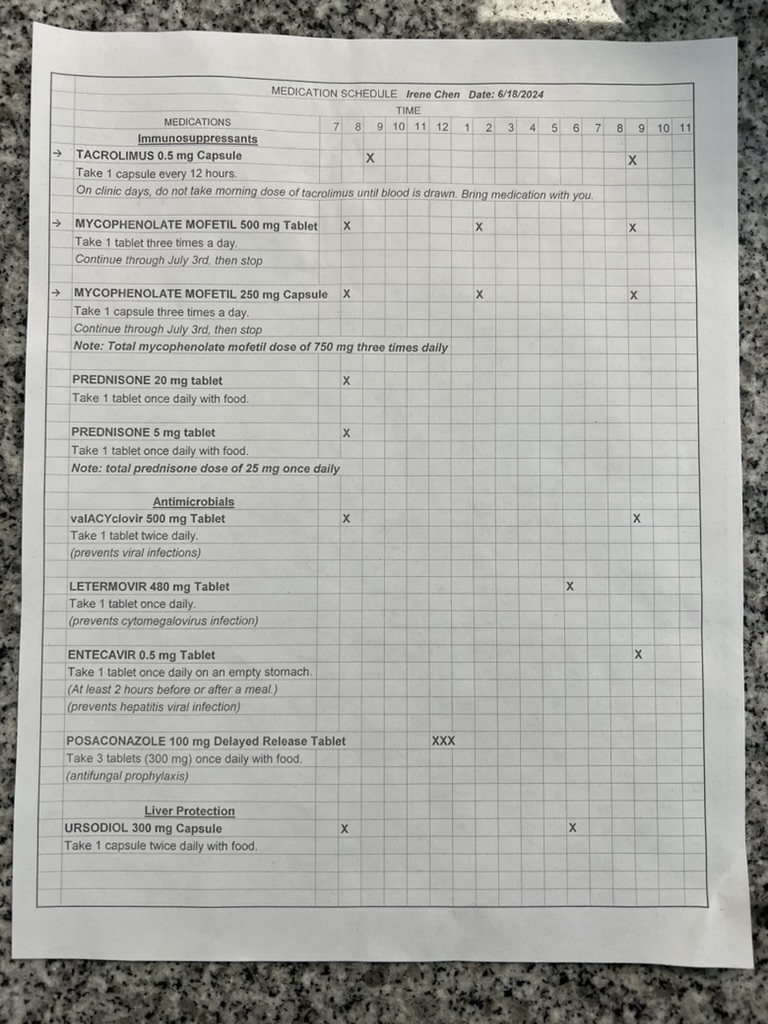
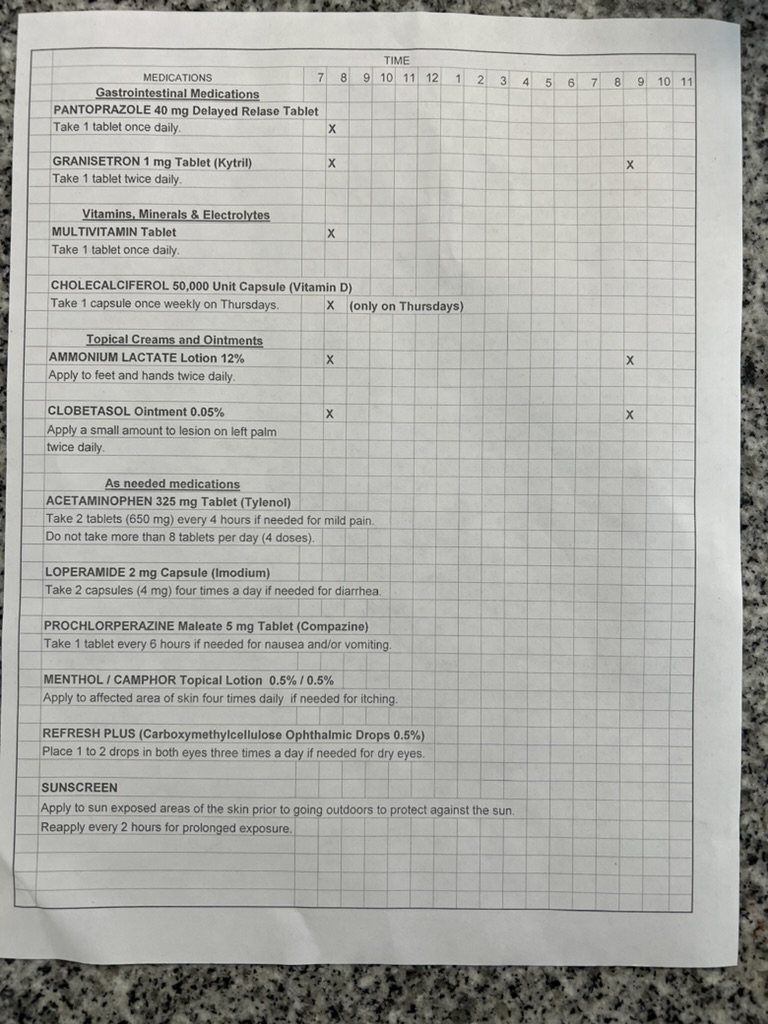
I had pharmacy teaching today with Tom the pharmacist – he made an amazing Excel spreadsheet with the drug names, times to take the medications, what the drug is for. The Excel sheet is speaking my language! Kudos to all you BMT pharmacists – thank you for what you do. I know there is so much behind the scenes stuff that you are all doing every day. The list of drugs is overwhelming and I don’t know how people who don’t have any medical background keep up on top of this. I have meds to take at 8am, 9am, 12pm, 2pm, 6pm, 9pm. It really feels like a full time job doing medications, eating meals, showering, putting on creams, walking, etc. I am so thankful for my family for helping me with all of these things.
Into the Wild
Now that I’ve engrafted though, I’m not necessarily out of the woods. The first 100 days post transplant are really critical and still quite scary. There are four main things to be nervous about during this time frame.
- Graft failure: there is always a possibility that the graft (Gordon’s cells) will be rejected by my body. This could in theory happen at any time in my life, but the highest possibility of this happening is in the initial 3 months post transplant. I am on steroids and other immunosuppressants that will help quiet my immune system and prevent graft failure, but the goal is to eventually taper off these medications slowly over the course of a year. While I won’t be able to tell symptomatically if I’m rejecting the graft, my medical team will be monitoring my blood counts regularly, hence needing to come into clinic 2-3 times a week for blood draws to make sure my numbers are trending in the right direction.
- Infections: Because I still only have a baby immune system, we are still concerned about infections: bacterial, fungal, viral. We are most concerned with reactivation of viral infections – things like CMV, EBV, zoster (aka chicken pox). These viruses live in everyone’s bodies, but because I’m immune compromised, they can reactivate and my baby immune system won’t be able to fight them off. We are prophylactically giving me anti-virals and anti-fungals, but they can always reactivate despite these measures. Symptomatically, if I did have an infection, I’d be looking out for signs and symptoms of infection like fevers, chills, etc.
- Graft vs host disease (GvHD): this happens when the donor’s immune system cells, called T lymphocytes, recognize the recipient’s tissues as foreign and attack them. This can cause inflammation in various organs, including the skin, gastrointestinal tract, liver, and lung. It’s most commonly seen in the skin and gut, so rash or worsening diarrhea are all in the realm of possibility.
- Organ toxicity from later effects of chemotherapy: While a lot of the effects of chemotherapy occur during the infusion or shortly thereafter, there are potential side effects from chemotherapy that happen months after. There may be possibility of liver damage so they will be checking my liver panels regularly. I may also get something called veno-occlusive disease (VOD) but am taking medications to help prevent that. Another effect from busulfan, one of the chemotherapies that I received, is known for is lung problems, specifically, cryptogenic organizing pneumonia (COP), idiopathic pneumonia syndrome, or interstitial lung disease. It’s all very scary and I could in theory all of a sudden feel shortness of breath that might not resolve over time. Let’s keep our fingers crossed that none of these things happen.
With this giant list of possibilities, I’ll be at an apartment in Bethesda nearby and going into clinic 2-3 times a week for blood draws and follow up appointments.
At day 28, we’ll also do a chimerism study, which basically looks at how many of the cells in my body are Gordon’s cells and how many cells of me are left. Ideally, we’ll want 100% of the cells to be Gordon’s cells and none of my cells, but the different lineages of cells that are made from stem cells come in at different times. I’ll likely still need some “help” from IVIG, blood transfusions, platelets during this time as the new “me” learns to accept Gordon’s marrow.
Upward and onward!
Good evening, Irene.
I hope you’ve had a good day. Thank you for sharing and being vulnerable; it helps me understand a bit of what it would be like to be in your shoes. I can’t imagine going through it, but I trust that God gives strength and grace when it’s needed. I’m thankful for that and that your outlook is both accepting (even with humor) and hopeful! You are an encouragement.
Hello to Gordon, too; I hope he is doing well. (I think I told you that my husband was a bone marrow donor, which isn’t easy though nothing like what you are enduring). Gordon has had a huge part in this.
I am very excited with you for your discharge. I hope you’ll have blue skies, trees and flowers and fresh air to greet you as you exit the hospital – stop, look and listen, and may every day bring a little more healing, even if it’s not a linear journey. Love to you. 🙂
Yay for a solid poop! You are making tremendous progress! With all the scary possibilities and all that this process demands of you, don’t forget to be gentle with yourself-I know overachiever Irene is probably feeling all the feels!
We love you SO much and are counting down the days until you have your shots and are back in Seattle so we can fly out there to give you an outdoor socially distanced and masked (air) hug!