The last few weeks have been somewhat of a whirlwind. I had a range of emotions the last two weeks in Maryland. I was obviously very excited to be going home, but I was also extremely nervous. The NIH has been wonderful in managing my care and I didn’t have to spend any mental load doing it myself – the primary BMT team would coordinate ALL of the logistics of my care. They would just tell me when and where to show up. I knew going back home meant that a lot of that coordination would fall onto me. Because the NIH doesn’t take insurance, there are no quotas on numbers of patients to see, and they can spend as much time as they need to address your concerns. If I had an issue, all I’d have to do is text the PA, Erin, and she’d tell me to come in that same day or she would coordinate for me to see a specialist. Unfortunately, this is not how things work with private insurance. Wait times are usually months to see specialty providers, even if you are already an established patient.
I had my last two clinic follow ups with the BMT team in August before I headed home to Seattle with my mom and dad.
BMT Clinic Follow Up (8/19) – Day 82
Today was a relatively short day in clinic with labs followed by a visit by Erin and Dr. Arnold. Some of my numbers are steady (WBC, hemoglobin, and platelets) but not quite normal, but my lymphocytes (T and B cells) have still not yet come in. We’re hoping by the 6 month mark I’ll be making them on my own. Fingers crossed!
I had a few more appointments the rest of the week with dermatology and endocrinology. The rash on my face is still there, but we’re using ivermectin cream to see if it’ll get better. With endocrinology, I’m still on steroids but I am finally down to physiologic hydrocortisone (what your body would normally produce). I’ll have to be on these for a while and continue to decrease the dose slowly. At some point, I’ll have to do a stimulation test to see if my adrenal glands are able to produce cortisol on their own, but until then, I’ll be taking them by pills.
BMT Clinic Follow Up (8/26) – Day 89
My last clinic day at the NIH with Erin and Dr. Arnold. They did tank me up with some IVIG as I’ll be getting on a plane later this week. I did also get to discontinue some of my antimicrobials – posaconazole (anti-fungal), entecavir (hepatitis B prophylaxis), and letermovir (for CMV prophylaxis) which was timed perfectly so that when I get home, I can get labs and make sure that my tacrolimus drug level is still at a therapeutic range.
After getting home from IVIG, we spent the whole day packing up.
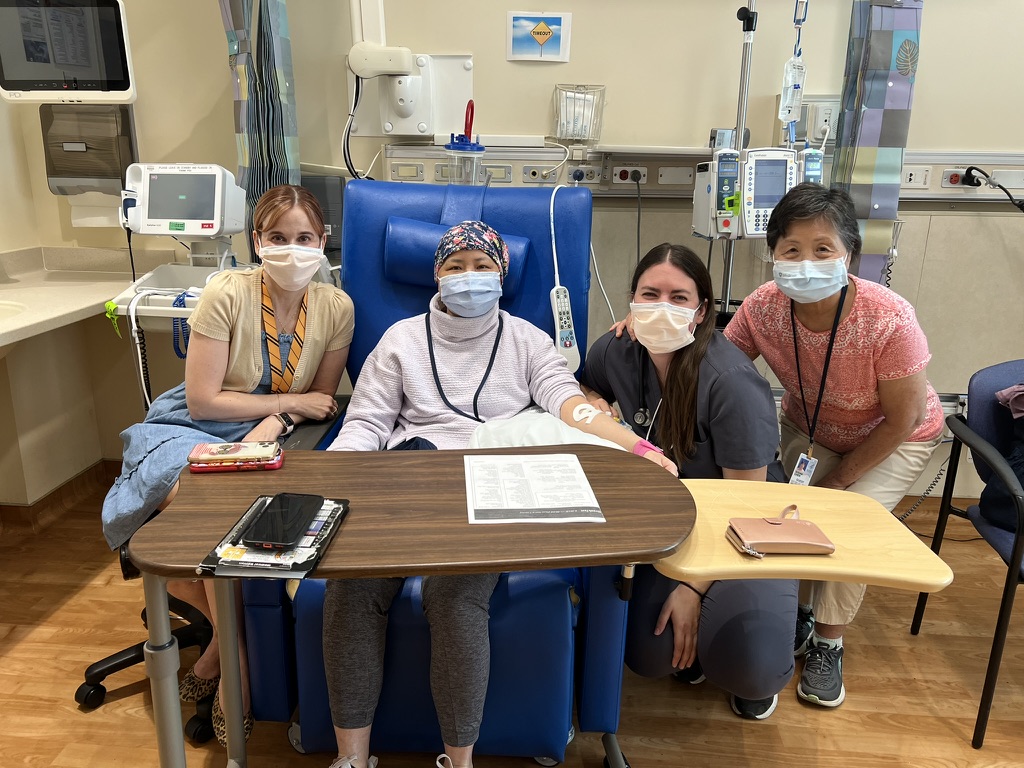


BMT Team at Fred Hutch (8/29) – Day 92
I met the BMT team at the Fred Hutch on Thursday when we got home. I had to get labs early in the morning followed by a pulmonary function test. I then met with the BMT team that included Kate (NP), Bianca (nurse), and Dr. Carpenter (hematologist/oncologist). The wonderful thing about Dr. Carpenter is that he’s pediatrics trained so he spends a good amount of time at Seattle Children’s Hospital and is familiar with primary immune deficiencies. The NIH sent a very thorough summary of my transplant course and we mainly discussed the issues I’m still struggling with: nausea, blurry vision, and fatigue. I got a referral to an optometrist that has a specialty in GvHD for transplant patients. We discussed getting vaccinated with COVID and flu which differed a bit from what my NIH team had suggested.
The main thing we discussed though was who was going to be the primary point for my care. For the local patients at the NIH, the BMT team continues to follow the patient every other week after day 100. After the 6 month mark, if the patient is doing well, they can space the visits out to monthly. I think the NIH team expected that the BMT team would be the primary point in managing my care. However, at the Hutch, after day 100, patients are sent home to their home oncologist. Unfortunately, I don’t fit into a “typical” patient journey since I have a rare disease that’s often diagnosed and treated in children. We decided that my immunologist, Dr. Chau, would be the primary point of contact and she would coordinate with Dr. Carpenter if any issues arose. However, because Dr. Chau works at Seattle Children’s Hospital and she cannot put in orders at UW, my primary care physician, Dr. Wright, would also be a point person in case I need orders to be put into the UW system. It’s honestly a cluster dealing with different institutions. You would think that these systems are all connected, but they are not.
The highlight of the week though was definitely Maple returning home. Forrest had some chairs set up in the backyard before we got there to make sure that Maple didn’t knock us over when she saw us. My mom and I had treats in hand to distract her from jumping on us, although that was still inevitable. We probably fed Maple way too many treats that afternoon, but it was well worth it. I have to say Maple was a little bit confused though over the next few days. I think the silence in our household was jarring to her as she’s used to having her best friend Neville to play with. We’ll have to do a reunion soon!



Labor Day Weekend (8/31-9/2)
The excitement of coming home really took a toll on me over the weekend though. Going up and down the stairs at my house to unpack was probably more exertion than I had done in the last several months. I also went on a walk with Beth on Friday down to the beach and had been taking Maple on walks two times a day to go potty. It doesn’t seem like much, but it definitely felt like a lot to my body. I realized after the weekend that my average step count over the time I was in Maryland was around 2,300 steps/day and just in the last few days at home, I had been doing 7-8K steps a day.
Because I likely overdid it, I ended up sleeping almost all of Labor Day weekend to recuperate. I could feel my muscles aching too so I did some bedtime stretches. It’s a little bit discouraging to see the level of fitness I am now compared to what it was before transplant, but I also know need to be kind to myself with the level of de-conditioning that I experienced being hospitalized for 35 days plus another 14 days. For every day you’re in the hospital, you can expect to take 3-5 days to get better once you’re out so patience is something I need to work on.
Immunology (9/4)
I saw Dr. Chau today at Seattle Children’s Hospital (SCH). It’s always funny when I check in at a children’s hospital and they ask “Are you the patient?” in a very confused manner. I had not been to SCH immunology in a few years and the new building that the primary immune deficiency team moved into is amazing! Children’s hospitals are much nicer than the adult side!
Our visit was over an hour as Dr. Chau is very thorough in all of our visits. We talked about the transplant, issues that I’m still having with transplant (nausea, fatigue, blurry vision), who is coordinating what, what referrals I still needed, what bloodwork/imaging/tests I need. Overall, a very long and overwhelming visit but much needed to establish the “new normal.”


Optometry (9/5)
Because I have been having blurry vision, I went to see an optometrist, Dr. Lam, at Eye Associates NW, who specializes in ocular GvHD. While I don’t have evidence of ocular GvHD, I do have extremely dry eyes so she gave me some steroid eye drops (loteprednol) and a nasal spray (varenicline). She said blurry vision is very common in post transplant, but the double vision is less common so hopefully the new prescriptions will help. She also noticed that my corneal nerve was pretty degenerated (neurotrophic keratitis) – she poked my eye and I barely flinched so that wasn’t a great sign. I’m waiting for insurance to cover a medication called Oxervate, that is supposed to help with degenerated corneal nerves, but who knows when I’ll have access to it. I’m due to see Dr. Lam again next month to see if there are any improvements with the blurry vision.
A day off! (9/6) – Day 100
I didn’t have any doctor appointments today, but my company car did get towed by a towing company since the battery died and the car wouldn’t start. Check one more thing off my list of things to close out with J&J.
The absolute highlight of my week was definitely going on a walk with Forrest & Neesha (and their littles Coco and Neville). Maple was ecstatic to see them, and we had a lovely walk to the beach and sat on the bluff and chatted about life. It was also a celebration of reaching my Day 100 milestone.


Labs (9/7)
Because my immunosuppression drug level (tacrolimus) has not been in the therapeutic range since I’ve been home, I’ve had to get labs twice a week while we’re still adjusting the tacrolimus drug dose. Since Dr. Chau is based out of SCH, I drove over there to get labs done on Saturday morning.
Internal Medicine (9/10)
I met with my primary care doctor today, Dr. Wright. I’ve been with her since I moved up to Seattle in 2018, and I feel like I always see her after a big health episode – she must think I’m a hot mess. I love that when she knew I was a complicated case, she said that she’d be available to see me when she can and that I would bypass all the residents that normally see patients at this clinic. She always spends over 40 minutes on my clinic visits, even though I know I’m slated to be there for 15 minutes only. She never rushes me and is very thorough despite knowing that she’ll be running behind. She’s always trying to make my life easier, and when I told her that SCH is somewhat far from my house and that some days it can take upwards of 45 minutes to get there, she put in lab orders for me so that I can go to a UW location to get them drawn.
She also referred me to home physical therapy since I’ve become so de-conditioned from my time in the hospital. I’m so grateful she’s on my care team!
Immunology (9/11)
For the next month or two, I’ll be seeing Dr. Chau and getting labs every week. Since my lymphocytes (T and B cells) still have not come in yet (womp womp), I’m still highly immune compromised and will need to be on IVIG for the foreseeable future. The good news is that we’re trying a significantly lower dose than pre-transplant (33g vs 70g) and we’re spacing it out more (every 4 weeks vs every 3 weeks). Hopefully I won’t feel as lethargic and crummy after IVIG days.
Oral Medicine + COVID shot (9/13)
Today was a post-transplant baseline check up with Dr. Dean at the oral medicine clinic at Fred Hutch (FHCC). I was actually seen in this clinic several times in 2022/2023 when my oral ulcers started and Dr. Dean was doing injections in my mouth. He had seen my mouth at its worst, so he was surprised today to see my mouth the best that it’s ever been. It’s still not normal – my tongue is still pretty denuded – but to see that there were no ulcers was a huge win.
Interestingly, FHCC recommends no dental work until 9-12 months post transplant and with prophylactic antibiotics, but the NIH team said it was fine to get my teeth cleaned when I got home. I’ll probably err on the side of caution moving forward and wait until my 9 month mark until I get my teeth cleaned again.
I had signed up to get a COVID/flu vaccine at Rite Aid after this appointment. The NIH team recommended I wait until the 6 month mark to get any vaccines, including flu and COVID, but the FHCC team recommended that I get these two vaccines as soon as they come out. They feel that the benefit of getting these (even if my lymphocytes are not in great numbers) outweighs the risk. I’m supposed to get the high dose flu vaccine because I’m immune compromised, but Rite Aid wouldn’t allow me since it’s usually for patients over 65 and insurance automatically rejected it. I’ll have to do this in clinic, but I was able to get my COVID vaccine. Insurance really does not work well for people who aren’t “normal.”
I spent the rest of the day coordinating care – calling Providence home infusion to see if the IVIG prior authorization went through, Providence physical therapy to answer the intake questions before I can be scheduled with a provider, calling Accredo specialty pharmacy to see if the Oxervate prior authorization was approved, calling the internal medicine clinic to schedule a high dose flu vaccine, calling SCH to see if the brain MRI Dr. Chau put in was ready to schedule. All of this coordination of care takes SO MUCH TIME. It truly is a full-time job – there was a patient care coordinator at the NIH who did all of this for me when I was there, and now, I’m that person.
The rest of the month is filled with more appointments – ID, pulmonology, GI, immunology, ENT, but hoping that October will be a slower month with a lot of rest.
Thanking God and celebrating day 100 with you! Woohoo! And I love seeing all the pictures of “home”!
Thank you!
Welcome home Irene!
Thanks!
Here’s to a restful and healing October!!!