Saturday, Monday, May 18, 2024
I have a 5 day break from chemotherapy after doing 3 days of Campath (alemtuzumab) on Wednesday, Thursday, and Friday. The weekends at the NIH are eerily quiet but it also means it’s a good time to get out of my room since there are barely any people in the building. Unfortunately, it is pouring rain all day today, so I wasn’t able to get to the real outside.
Unfortunately, I wasn’t feeling that great this morning. I woke up with some light chest pain and the feeling like my heart was pumping out of my chest. My blood pressure was also high in the 140/90s.
Because of all of this, I decided to take it easy today and just take a walk around the floor when I was feeling up for it, but for the majority of the day, I stayed in bed and took naps. The team did put in orders to do a whole workup so I ended up getting a chest x-ray and EKG today and they’ll schedule an ECHO and pulmonary function test later in the week.

The EKG was normal and the chest x-ray had noted a nodule on one of the lobes of my lung, but prior chest CTs have shown scarring in my lungs from old infections so it’s likely nothing.
My nurses today were wonderful. Andreas took care of my in the morning and Sujung was my night nurse. Andreas and I had a good heart to heart talk about life. He has an interesting story in that he did part of nursing school in Spain, but ended up moving back to the states to finish his Bachelors in Nursing. He’s been on the BMT floor for the last 7 years and we got to talking a lot about faith and how he’s able to maintain a strong belief even while working on a unit like the bone marrow transplant floor where there’s so much suffering. Life seems just so unfair. Being that person who always strives to do the right thing and makes the right choices, but being handed this deck of cards of constantly being sick, the idea of religion has been a big struggle for me. I do always enjoy the conversations, but I’m still not sure where I stand.
Sunday, May 19, 2024: Day -10
Andreas was back this morning and it’s nice when you get to see the same nurses a few days in a row because you kind of get into a groove of how they operate and they learn what your preferences are.
The campus was completely dead today, so my brother, mom and I were able to go outside for a walk today. It was nice to get some fresh air, but because it had rained all day Saturday, there were lots of mosquitos and gnats outside because of how humid it was. The highlight was definitely seeing the little pods of geese – three families with their babies.



Patricia was my night nurse and I learned that her daughter just finished her PhD in Davis, CA in anthropology. We had a long heart to heart talk about life which was nice. I have to say that all the nurses here have been wonderful. I think because their ratios are 2 patients to 1 nurse, they’re actually able to get to know their patients and truly take care of them. Their nursing skills are also really top notch. They are very diligent about scrubbing the caps of all IV lines, especially the central line, for at least 10 seconds (Danielle – I’m thinking about that time I yelled at the ER nurse in Portland). They’re very diligent about changing their gloves if they touch a doorknob or the floor. It really is the little things to make sure patients on this floor don’t acquire other infections while we’re here. It’s SO appreciated, coming from someone who has acquired many hospital acquired infections (C. diff, norovirus, pneumonias, etc.)
Monday, May 20, 2024: Day -9
Andreas (morning) & Patricia (night) were here again today! Today was a BUSY day though. I don’t think I was in my room for very long at all.
7:00 AM: Pulmonary function test
My last PFT test showed me desaturating down to 88% when doing a 6 minute walk test. They wanted to repeat it to make sure I wasn’t actually desaturating. Luckily, it seemed like everything was fine so hopefully the last test was just a fluke.
9:00 AM: tacrolimus lab draw + morning medications
Since I stopped taking posaconazole (anti-fungal) orally, my tacrolimus levels have been low (there’s a drug interaction with these two meds that makes the tacrolimu level higher). Tacrolimus is an immune suppressant that I have been taking since December because my body for whatever reason has been giving me mouth ulcers. With this medication, it has to be in a certain therapeutic range in your body so we have to draw levels to make sure it’s in an acceptable range.
10:00 AM: Pentamidine inhalation
I had to go back down to see respiratory therapy for a pentamidine inhalation. One of the infections that immune compromised people can get is Pneumocystis pneumonia, also known as PJP or PCP. While Bactrim or dapsone are some oral medications that can be taken to help prevent this, my team is transitioning me off oral medications in the event that I get terrible oral ulcers during chemotherapy that I’m unable to eat. Hence, another option to treat or prevent PCP is an inhaled antibiotic called pentamidine that I would do once a month. The crummy thing about this drug is that you have to sit in a hood and breathe into the hood for 15 minutes while the medication goes into your lungs. The medication tastes like metal and makes your mouth and throat super dry so it made me want to cough a lot. Luckily, I got to eat some candy afterwards.
1:00 PM: Recreation therapy
I started to request doing recreation therapy with Amber and Isabell (the intern) which is basically either arts and crafts or going to the gym. Can you guess what I chose? My doctors signed off an order to allow me to use the gym before I become severely neutropenic; however, I’m only able to use the bike and not the treadmill for fear of falling. I was able to use the stationary bike for about 20 minutes, and I’m trying to be kind to myself, but it is really challenging sometimes for me to think what I was capable of now vs what I was capable a year ago vs what I was capable pre-2022 (orange theory & tennis 3-4 times a a week). I guess comparison is the thief of joy, so I should just be focusing on what I can do now, rather than what I cannot do.
2:00 PM: Chest CT
I got a chest CT to finish the workup from my weird palpitation episode on Saturday. Nothing exciting came of this, but boring is good.
3:00 PM: Mycofungin
IV antifungal prevention
4:00 PM: Dr. Arnold
Dr. Arnold is my assigned transplant provider. She is a badass and I just love her so much. While I don’t see her everyday (the rounding team is who I see on a daily basis), they do provide updates to her and she’ll come visit me every few days to just see how I am doing. It ended up being more of a social visit, but can we be friends?!?
Tuesday, May 21, 2024: Day -8
6:00 AM: lab draws
I’m definitely not a morning person so these 5/6 am lab draws are my worst nightmare. Luckily, they are so kind and I can usually sleep through it while they take vitals and do all the things.
7:30 AM: Tonya
Tonya popped her head in this morning to make sure I was doing okay after the weekend. She then goes back to report to the broader team, including Dr. Arnold on zoom rounds before the inpatient team rounds.
8:00 AM: ECHO
They were wrapping up the full workup from my palpitations from the weekend. My ECHO was all normal. Boring is good.
9:00 AM: tacrolimus lab draw + morning medications
10:00 AM: Team Rounds
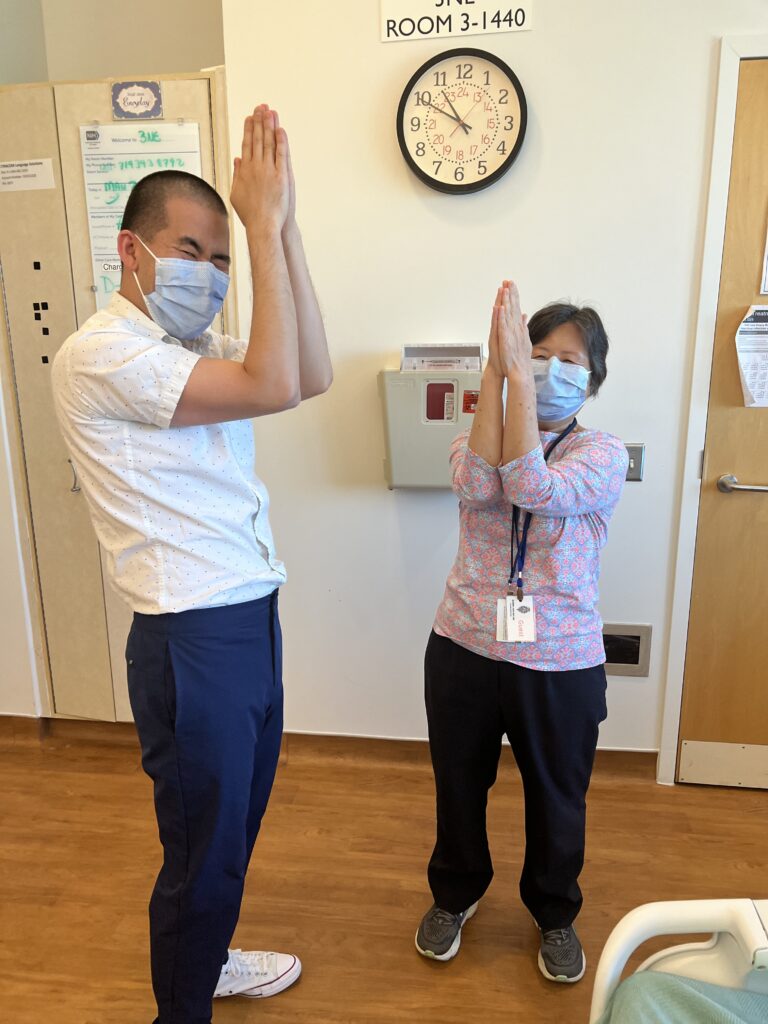
11:00 AM: Family Fun
I’m not sure if it’s really family fun, but after the inpatient team rounds on me, I usually will go on a walk or do some sort of activity. Today was a 15-minute arm workout. It doesn’t seem like it’d be that hard, but god damn – try this out and tell me you’re not in pain by the 3rd move.
1:00 PM: Mycofungin
Daily IV anti-fungal prevention
2:00 PM: Recreation therapy
Amber came to take us to the gym again! I did a 25 minute stationary bike workout and some weights for about an hour. There are 12 patients on the transplant floor, and I’m so curious because I’ve never actually seen another patient out of their room walking around. I curiously asked my nurse, my recreation therapist Amber, and Dr. Arnold the last few days, “What is everyone else doing and why haven’t I seen anyone else walk around?” I’ve gotten answers like “most people aren’t Type A like you” or “not to generalize, but the guys between 18-40 will sometimes bring their entire gaming console in and play for the 5-6 weeks they’re here” or “Pediatric patients are much easier to convince, especially since the adults are responsible for them, but adults are really hard to convince because we can’t make them do anything.” Everyone has said that those who stay active during transplant generally do better, so I’m going to try and keep going while I can because I cannot sit still, which is not surprising.
3:00 PM: Central line dressing change
They change the dressing in my neck every week to help prevent infection. It was nice to get the blood cleaned up a little bit. It’s a little red and slightly painful (1/10) but I think it’s because it got touched and there are 2 sutures holding it in place.

9:00 PM: evening medications
Alexis was my morning nurse, and Galina was my nurses in the evening. Galina is from Russia and interestingly enough, I learned that the people of Russia actually like Putin. I’m not sure why I was surprised, but I was.
Wednesday, May 22, 2024: Day -7
Alexis was my nurse again this morning. I think I’m staring to feel a little anxiety about what’s going to happen tomorrow.
6:00 AM: labs
8:00 AM: Tonya (NP) rounds
9:00 AM: tacrolimus level + morning medications (tacrolimus 4 mg, valacyclovir 500 mg, vitamin D 5000 IU, magnesium oxidde 200 mg, prednisone 25 mg)
I’m still falling behind on my tacrolimus levels since stopping the posaconazole so they keep increasing the tacrolimus dose. I’m not sure if it’s making my tremors worse, but I’m definitely very frustrated with having tremors.
10:00 AM: rounds with Dr. Dias, Tonya, and Dr. Fan
Dr. Dias has been on inpatient service since I got here last Tuesday and today is his last day before they change to a different attending. He has been so kind to me, visiting me multiple times a day. The entire team knows that I’m a pharmacist and that my brother is a physician, and I think there is an extra level of “take care of your kind” in situations like this. Dr. Dias and I had a lovely conversation the other day about pharma and life and how he loves working at the NIH because he really gets to spend time with his patients. He had previously worked at Dana Farber and other big name institutions, but having to deal with insurance and see so many patients and have expectations to publish a certain number of journals a year can be very draining in academia. I told Dr. Dias that when I go to ASH in 2025, I’m going to come find him and take a better picture. I am so truly grateful for the team.


11:00 AM: Family time
I forced Gordon to do a 15 minute leg workout video with me.
12:00 PM: Recreation Therapy
1:00 PM: Mycofungin
2:00 PM: Keppra & clonazepam
I start busulfan chemotherapy tomorrow, and one of the potential side effects of this chemotherapy is seizures. These two medications are to help prevent this.
3:00 PM: peripheral IV placement for PK draws tomorrow
Tomorrow’s dose of busulfan is also a test dose 4 am and it lasts for 3 hours. They have to draw something called pharmacokinetics labs at 7 am, 8 AM, 9AM, and 11AM. The reason for these blood draws is to see how my body processes the drug so that they can adequately calculate the appropriate dose of busulfan to give me for the next 3 days. Unfortunately, they cannot use the same line from my neck that they’re giving me the drug in to draw the PK values so I had to get another IV line started. Being in the hospital really makes you feel like a pin cushion. No fun at all.

4:00 PM: therapy because this shit is stressful.
6:00 PM: Magnesium oxide
7:00 PM: vitals & dinner
My blood pressure is absurdly high right now – 150/90 and it’s unclear. Is it the tacrolimus? Is it my lowered hemoglobin? Is it my anxiety about what’s to happen tomorrow? Is it because I know too much about this whole process? Who the heck knows. All I know is that this doesn’t feel good.
9:00 PM: evening medications (tacrolimus 4 mg, valacyclovir 500 mg, entecavir 0.5 mg)
12:00 AM: evening vitals
Hopefully when they come in a few hours, I’ll have calmed down. This is the last day where they will let me “sleep in” and do vitals every 6 hours. Because I’m starting chemotherapy tomorrow, they’ll be starting vitals every 4 hours which means sleep when I can because I won’t be getting much of it.
Tomorrow’s plan starts at 3 am with premedications (keppra, clonazepam, zofran, dexamethasone) so here we go.
Boniface is my nurse tonight. I’ve already expressed my anxiety about what’s to come in a few hours and he’s been very kind about everything to try and calm me down.
In other news, my peonies are blooming and my yard looks amazing (thank you Cameron and Katie). It’s just one less thing to have to think about while I am gone. Please come make a peony bouquet for yourself if you’re in the area. Someone should at least enjoy them if I can’t.


